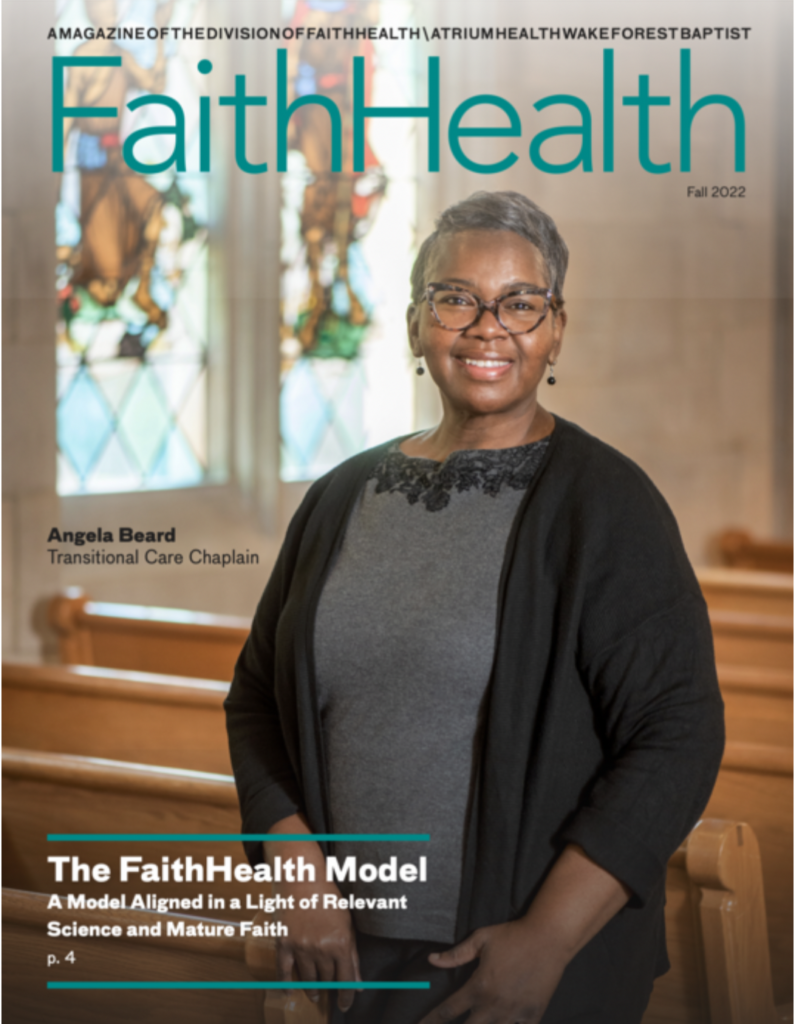
First Responder Chaplains (from left) Dana Patrick, Glenn Davis and Aaron Eaton talk with first responders.
By Tom Peterson
As the name implies, first responders are often the first to reach the scene of a trauma.
In the course of a normal week, they may have to deal with homicides, suicides, accidental deaths or the use of deadly force. They often deliver traumatic messages, including death notifications. Many are exposed to line-of-duty death. These high-level sensory exposures and other work-related tasks can lead to health challenges such as chronic stress, social isolation, suppressed immune system, anxiety or hypertension — all of which can contribute to poor health and shorter lifespans.
To address these concerns Wake Forest Baptist Medical Center (WFBMC) created a team of first-responder chaplains to serve fire, EMS and law enforcement agencies. The chaplains also work with campus police, hospital security and others in Forsyth County. It’s a large community, adding up to more than 3,000 first responders, not to mention their families and loved ones.
The program began in July 2016 when WFBMC brought the Rev. Glenn Davis onto its Division of FaithHealth staff. A 26-year chaplain for the Forsyth County Sheriff’s Office (FCSO), Davis had also informally served other area agencies. A service agreement between the FCSO and WFBMC created this much-needed countywide network of chaplaincy support, wellness education and crisis intervention services for the area’s most at-risk public servants.
“There’s something wrong if we just went out and dealt with victims of crime or domestic violence but we didn’t care for the people who are responding to them,” Davis says. “They’re not going stay in it long. The beneficiary of caring for responders are the communities they serve.”

A team of three
Davis now leads a team of three, which also includes Rev. Dana Patrick, a full-time staff chaplain, and Rev. Aaron Eaton, a second-year chaplain resident assigned to the program as part of his Clinical Pastoral Education training. Their duties include support during crisis intervention and support for families of those affected, death notification, and crisis response training for congregations. The group splits the responsibilities and coverage so there’s a presence in the sheriff’s office, the hospital, or ready for deployment into the community at any time.
That the chaplains are “embedded” with the first responders makes a big difference, Davis says. “Showing up and building trust before something bad has happened makes it more likely we will get turned to when something does erupt.”
Dealing with trauma
Trauma hits all of the senses.
“Even if you were just a visitor at the hospital, you could witness something that could be disturbing enough to partially incapacitate you or impair your ability to return to work,” Davis says.
 The chaplains provide crisis intervention, not counseling, but they are on the lookout for those who may need counseling.
The chaplains provide crisis intervention, not counseling, but they are on the lookout for those who may need counseling.
“People who have a healthy support system recover quite well from trauma,” Davis says. “But you hear people say, ‘I have no pastor’ or ‘I have relatives but don’t know where they are.’ Those kind of statements paint a picture of a person already in a vulnerable place before a traumatic incident ever happened.”
The team refers those people to talk with a pastor or to a counseling service.
Even with the disturbing images he has encountered, Davis is reminded of “how resilient the human spirit is and how people do have post traumatic growth. We come away with so much knowledge and insight from having suffered with people, and we’re changed by the mystery of that.”
There for the community
The chaplains are also ready to serve the larger community. Davis talks of going to calls crowded with whole waves of people.
“Sometime later,” he says, “you look up at a kitchen table or on the front porch and you realize 30 minutes ago this house was filled with chaos: five people looking for a suicide note, people taking pictures and others interviewing people, the hoard of neighbors. You may be there with just one family member or a handful of people. The world’s been rocked here. Something about the presence of a chaplain somehow honors that space, and you’re the last person to leave.”
 One of Dana Patrick’s first solo calls led her to a scene where a young woman had died of a drug overdose. During the holidays, she wanted to check in on people who had recently lost someone, she says.
One of Dana Patrick’s first solo calls led her to a scene where a young woman had died of a drug overdose. During the holidays, she wanted to check in on people who had recently lost someone, she says.
“So I called the mother of this overdose victim and left her a message letting her know that if she needed anything to get back with me. She called me back the next day in tears and said, ‘I’m so glad you called because today I just completely lost it and didn’t know what I needed to do.’”
Patrick says she was able to offer her some follow-up care for one of the most difficult of times after a loved one has died.
Right after that conversation, Patrick happened to bump into the investigator who covered that case and was able to provide the investigator an update on the family. “It was a nice closed circle, offering the follow-up care, being able to connect with both the law enforcement person as well as this family,” she says.
“The better we care for our responders, the better they are equipped to care for the community,” Patrick says. “It helps us to better care for the community’s most vulnerable.”